Updated 2023 guidance from the American Academy of Pediatrics (AAP) recommends drugs and surgery for children as young as 12 and 13 years who are struggling with obesity. According to new guidelines, middle school and high school age youth should be assessed and treated promptly and aggressively with use of medication for 12-year-olds, and surgery for those ages 13 and up.
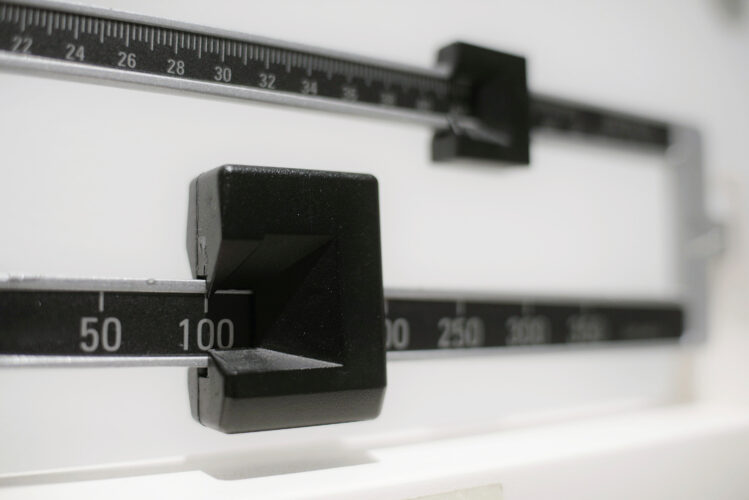
Roughly 20 percent of American children and teens are affected by obesity, according to the CDC. Having a body mass index (BMI) that meets or exceeds the 95th percentile for peers of the same age and gender qualifies one as obese while severe obesity is characterized by reaching or exceeding the 120th percentile.
According to updated guidelines, physicians should offer obese adolescents 12 and older access to applicable drugs and teens 13 and older with severe obesity referrals for weight-loss surgery, though circumstances may differ.
Dr. Sandra Hassink, medical director for the AAP and co-author of the new guidelines believes there is an inaccurate view of obesity as “a personal problem, maybe a failure of the person’s diligence.”
“This is not different than you have asthma and now we have an inhaler for you,” Hassink claimed.
Aaron Kelly, co-director of the Center for Pediatric Obesity Medicine at the University of Minnesota says, “Obesity is not a lifestyle problem. It is not a lifestyle disease. It predominately emerges from biological factors.”
Contrary to these statements, other doctors find the claims curious as this “genetic disruption” in human evolution is something that has only just developed in the past few decades with a coincidental acceleration with pandemic lockdowns.
Following the AAP’s recommendations to include surgery and medication to combat childhood obesity, Dr. Marc Siegel and Dr. Nicole Saphier suggested many solutions and mitigation tactics to reduce the affliction.
Siegel believes the new guidelines are responding to an “emergency” worsened in part by COVID shutdowns of schools and an overall increase in sedentary pandemic activities. He added that while the rates of childhood obesity jumped to 20 percent from five percent back in 1978, that number “exploded” particularly in the past two-and-a-half years.
Dr. Saphier cited that cultural factors impact these numbers even more than the effects of the pandemic.
“There’s been a pervasive culture when it comes to talking about people being overweight. All of a sudden, physicians are being told they can’t use the terms obese and overweight; mind you, these are medical terms,” she said.
Saphier alleges that pop culture practically “celebrates” being overweight and obese, citing pop star Lizzo, a leading spokesperson of the body positivity movement whose size is glamorized in the media.
“Being bigger is unhealthy, and there are consequences to being bigger,” she added.
One of Dr. Siegel’s top concerns is the lack of knowledge the medical community has garnered regarding childhood weight loss surgery and medications that are typically prescribed for adults.
“We don’t know the long-term implications of doing this to children,” he said.
Ozempic and Tirzepatide are two medications formerly only offered to those afflicted with type 2 diabetes and works by boosting the body’s production of insulin and reducing the amount of glucagon.
While Siegel admits the drugs have been wildly effective in decreasing people’s weight while essentially simulating bariatric surgery without the necessity for the actual operation, he cautions there are no long-term studies to determine how the drugs affect children’s gut hormones, recommending against them for anyone under the age of 18.
In agreement with Dr. Siegel, Dr. Saphier said that surgery and medication can be good possibilities for people who have failed endlessly to live a healthy lifestyle but should only be contemplated after all other options have been exhausted.
“Americans, in general, are always looking for the quick fix,” Saphier said. “We want a pill, a quick diet, anything that could give us a positive outcome with minimal effort, and unfortunately, that’s created our society.”
Both experts recognized healthcare disparities in socio-economic groups exacerbated by government-allocated resources meant to help poor Americans, but end up harming Black, Hispanic and non-White households more commonly observed in lower tax brackets. One example Dr. Siegel cited was how food stamp programs include several unhealthy processed foods that are too high in sugars, carbohydrates, sodium, and unhealthy fats.
“While I don’t necessarily love increased regulation, when it comes to spending tax dollars, I think it is essential that this money is not going to unhealthy treats that will have long-term consequences,” Dr. Saphier added in agreement.
She proposed the concept of a tax incentive for those buying healthy whole foods and a higher tax on unhealthy foods that could be allocated towards obesity-related chronic illnesses, which costs $173 billion a year.
Both Dr. Siegel and Dr. Saphier urge families afflicted with obesity to work with their pediatricians to assist with constructing health plans targeting nutritious food intake and physical activity.
“It sounds harsh, but I do think parents should be held accountable for their children becoming morbidly obese,” Saphier said. “I think it is a form of child abuse, and we cannot tolerate it.”












Add comment